Key Messages: Act Swiftly – Test, Trace and Contain the Spread
-
Be proactive and act swiftly to get ahead of the curve to stop the spread
-
Enhance basic public health measures throughout to eliminate transmission
-
Scale up testing, contact tracing and targeted quarantine at speed, to minimise avoidable harm to health, civil liberties and the economy
-
Strengthen global co-ordinated responses now and for the future
Key Principles:
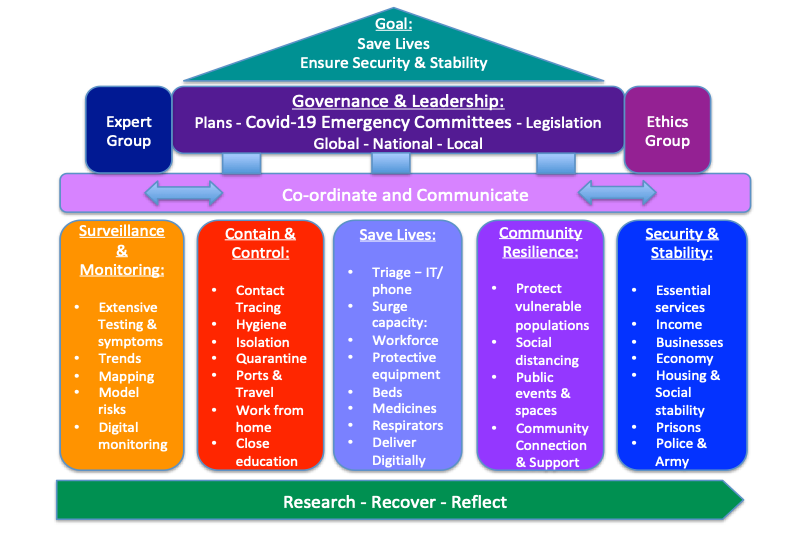
Take it Seriously: Demonstrate courageous leadership, and establish global, national and local emergency committees to oversee strategic responses as below:
Coordinate and Communicate: Ensure clear lines of co-ordination between sectors and geographical levels, and establish daily communications supported by social media
Stop the Spread: Prioritise testing and surveillance to monitor and target proportionate responses with basic public health measures to control and contain the outbreak
Save Lives: Prepare surge capacity of the health sector, with triage systems, re-deploy staff and buildings supplied with protective equipment, beds and respirators
Protect and Secure: Create caring communities, target and protect vulnerable populations; stabilise economic impacts, ensure essential services and wider security
Research, Recover and Reflect: Fast track research prioritising vaccines; establish a Recovery Committee for long-term planning; evaluate and reflect for the future
An Emergency Framework for Countries and Communities – for COVID-19:
Overarching Goal:
Is to save lives and protect vulnerable populations, nationally and globally, whilst minimising inadvertent harm to social and economic disruption and human rights, as well as progress on delivering the Sustainable Development Goals.
Global Responsibilities re the Pandemic:
- UN and Multilateral Emergency Responses - Strengthen global emergency co-ordination with increased multi-sector leadership, planning, communications and funding – supported by a co-ordination council with links to the UN
- Reduce Risks – of a potential reversal in sustainable development, a global economic recession, increased civil unrest and conflicts and threats to global security
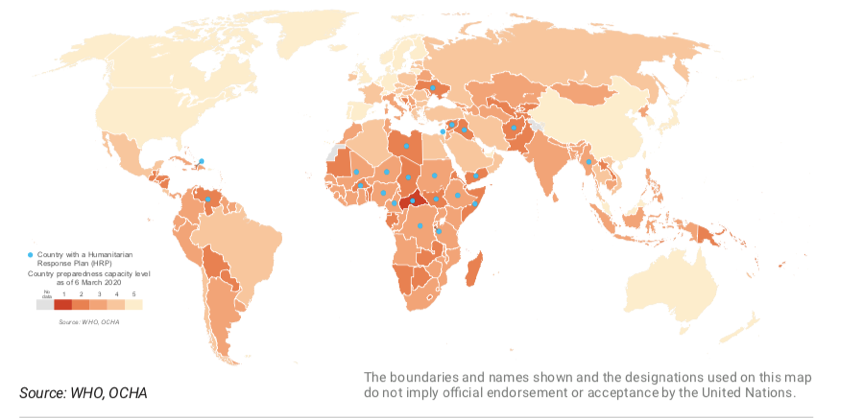
- Prioritise Stopping the Spread - Informed by basic public health interventions, including enhanced testing and surveillance, combined with control and containment measures, especially in countries and communities that have limited health systems to respond
- Collaborative and Co-ordinated Action – Provide multi-sector responses to enhance capacity at speed and scale, with resources, tests, equipment and staff; and share learning across countries as the pandemic spreads
- Ethics and Equity - Apply an ethical framework to balance rights with responsibilities and minimise overall harms including the relative impacts upon disadvantaged populations; embed gender equity across governance and delivery processes
- Establish Recovery Responses – to build back green and to create a sense of hope for the future, whilst reducing negative impacts upon achieving the SDGs, and strengthen health systems in responding to future emergencies
- Invest in Research and Evaluation – to identify effective treatments and bring forward a potential vaccine, the effectiveness of current responses and to prevent the spread of future pandemics
We are only as strong as our weakest health system:
https://www.un.org/sites/un2.un.org/files/sg_report_socio-economic_impact_of_covid19.pdf
Country and Community Responses:
- Take it Seriously - Establish Emergency Committees:
Political Leadership: As this has now been declared a Pandemic, which risks everyone across the world, courageous leadership is required at the most senior levels in government. Declaring a national emergency and establishing national and local emergency committees to oversee the development and implementation of an emergency plan based upon scientific and expert advice; put in place appropriate and responsive legislative powers; and establish an ethics group to advise on competing priorities going forward. A key role of the Emergency Committee is to ensure clear lines of responsibility and reporting across government sectors and the private sector to ensure a co-ordinated response and to communicate key messages daily.
Emergency Plan: Be proactive and strategic in addressing the pandemic - and develop an overall plan with a goal, guiding principles, governance arrangements, co-ordination and delivery mechanisms, and a communications strategy. Undertake a rapid risk assessment in order to anticipate and manage hazards in advance and embed mitigation efforts into the planning process. Identify key triggers to move from one stage of the plan to the next and draw upon the World Health Organisation guidance as well as lessons from other countries. https://www.who.int/docs/default-source/coronaviruse/srp-04022020.pdf?sfvrsn=7ff55ec0_4&download=true
Legislation: Build upon existing Public Health Acts, and National Security and Emergency Legislation; develop rapid amendments to provide the necessary political powers to control the Covid-19 epidemic through the different stages of the plan. Ensure a balance of rights with responsibilities, whilst protecting vulnerable populations; provide a clear rationale and justification that are communicated to the general public.
Examples of emergency and public health legislation from the UK:
http://www.legislation.gov.uk/uksi/2020/129/contents/made
Expert Groups: Establish expert groups to inform the National Emergency Committee as well as public facing communications messages. From the Health Sector perspective, expertise can draw upon international evidence and advisors from the WHO, as well as national experts in health service delivery, emergency planning, infectious disease control, modellers and virologists. Additionally, establish a multi-sector expert group, covering public and private sectors as well as security, in order to develop a tailored risk assessment and contingency plan for the national committee.
Ethics Group: Establish an ethics group at national level to draw up guiding principles for dealing with conflicting priorities and limited resources in health and care settings and across the key aspects of the emergency plan and legislation. The Ethics Committee can also be engaged in advising communications messages to ensure balanced messages are given between protecting rights with our responsibilities to prevent harm to others.
Gender and Equity:
- Ensure a balance of Gender and Diversity across the decision and governance processes, including Emergency Committees, Expert and Ethics Groups
- Embed gender and equity analysis and responses across legislation and plans to ensure inadvertent harm to vulnerable populations at all levels
Co-ordinate: Establish a mechanism to ensure multi-sector co-ordination across key public and private services involved in responding to the national epidemic, in order to deliver the national plan or strategy. Ensure clear roles and responsibilities are identified, along with lines of accountability and decision making. Communicate clearly across the system definitions, goals, rationale and principles for each stage of the plan.
Lessons from China: A co-ordinated response
A clear strategy was developed, and goals were well articulated and communicated across the entire response architecture. This strategy was rapidly adapted and adjusted to the outbreak, both in terms of the epidemiological situation over time and in different parts of the country.
The epidemiological situation has been used to define location into four areas:
- In areas without cases, the strategy in these areas is to “strictly prevent introduction.” This includes quarantine arrangements in transportation hubs, monitoring for temperature changes, strengthening of triage arrangements, use of fever clinics, and ensuring normal economic and social operations.
- In areas with sporadic cases, the strategy is focused on “reducing importation, stopping transmission and providing appropriate treatment.”
- In areas with community clusters, the strategy is focused on “stopping transmission, preventing exportation, and strengthening treatment.”
- In areas with community transmission, the strictest prevention and control strategies are being implemented, the entry and exit of people from these areas has been stopped and public health and medical treatment measures are comprehensively strengthened.
The “Lessons from China” boxes are drawn from the WHO-China Joint Mission on Coronavirus Disease (COVID-19) in February 2020 – to provide early learning from the first country to deal with the outbreak.
Communications: Develop a communications strategy to match the stages of the national plan, including internal communications to facilitate coordination. Include daily multimedia communications responses for the general public, providing key messages about the nature of the infection, how to protect themselves and their families, the rationale for the national plan and responsibilities to others in their community to save lives.
Messages from political leaders helps to convey the seriousness of responding appropriately to control orders. Additionally, regular communications about the national plan, its implications and future steps allows communities and families to feel as stable and secure as possible and make appropriate arrangements as the process unfolds.
Communicating a sense of pulling together for a common good, as well as emphasising aspects that are protective, enhance resilience and bring out the best in people, are key to a good media campaign, including conveying a sense of calmness and security.
Going forward, providing a clear plan and rationale for different responses will give a sense of certainty in what can be felt to be a chaotic process. Actively communicate positive messages of hope and inspiration about compassionate community responses.
Key Facts re COVID-19
The Coronavirus: The Coronavirus COVID-19 comes from the same family of viruses that cause the common cold. COVID-19 is thought to have originated by a mutation in an animal (possibly bat), that then passed to humans, probably within the Wuhan animal market, where an atypical pneumonia was first detected in December in China, 2019. The virus has spread rapidly in our globalized world, and the World Health Organization declared a Pandemic on the 11th March, which has since spread to virtually every country in the world.
Clinical Manifestation and Progression: the incubation period is between 1-14 days, most commonly around 5 days. The most common symptoms include fever, fatigue and a dry cough. The below outlines the range of symptoms that can be experienced as the illness progresses:
- In the first 1-4 days - symptoms are similar to a regular cold, with a mild sore throat and occasionally some diarrhea and nausea and a headache;
- After 5-6 days - symptoms progress with an increasing sore throat, a low fever and chills, aches and pains and the development of a dry cough and difficulty breathing;
- By 7-9 days - symptoms become increasingly worse, with a higher fever, a feeling of exhaustion, with a sense of heaviness in the chest and shortness of breath, the dry cough can become productive and in some, worsening symptoms of diarrhea and vomiting can occur. It is at this stage that patients can develop pneumonia with symptoms potentially becoming rapidly worse due to respiratory failure.
- Symptoms requiring urgent treatment - include difficulty breathing, pains in the chest and bluish lips or face, as this may indicate progression of pneumonia with respiratory failure. Patients should be sent urgently to hospital.
- Recovery - most mild to moderate cases take 2 weeks to recover, whilst the majority of severe and critical cases take 3-6 weeks to recover.
Outcomes:
- Mild - Moderate: 80%
- Severe: 14%
- Critical: 6%
- Fatal: 1-3%
From experience in China, the majority of cases are mild to moderate (approximately 80%), though worse than a common cold, mild cases do not develop a pneumonia and do not always have a fever and can be treated and recover at home. Whilst moderate cases experience a cough with shortness of breath. Mild and moderate cases can suddenly deteriorate into severe or critical, after about a week of symptoms. Approximately 20% of all cases are classed as severe or critical and develop pneumonia that requires hospital care with oxygen. Approximately 14% of cases are classed as severe and experience respiratory distress, whilst 6% experience a critical illness with respiratory and multi-organ failure and require a respirator and intensive care. Fatality rates appear to be minimized with earlier intervention and range from approximately 1-3%.
Demographics: Analysis from the outbreak in China found the median age is 51 years (range 2 days-100 years old) with the majority of cases (77.8%) aged between 30–69 years. Data on children aged up to 18 years suggests that there is a relatively low attack rate in this age group (2.4% of all reported cases). In an investigation of 147 pregnant women (64 confirmed, 82 suspected and 1 asymptomatic), 8% had severe disease and 1% were critical. Populations with higher rates of older and vulnerable people will experience the epidemic differently, as their risk of death was found to range from 5-20%. Vulnerable groups include those over 60, males, people with underlying conditions including hypertension, diabetes, cardiovascular disease, respiratory disease and cancer. Obesity and smoking have also been identified as risk factors.
How it is spread: COVID-19 is transmitted via droplets from an infected person from respiratory secretions, including coughing and sneezing and subsequent contact with infected surfaces. Metal and hard surfaces can stay contaminated for approximately 2-3 days. Airborne spread has not been determined as yet for COVID-19, however it may be a factor in its rapid transmission, along with droplets, from breathing, speaking, sneezing and coughing. In China, human-to-human transmission of the COVID-19 virus has largely occurred in families.
Period of infectivity: although further research is required, initial small studies indicate that individuals may be infective a couple of days before they develop symptoms, and that they are mainly contagious in the first week on the illness. Initial findings suggest that after an individual develops antibodies by about 10 days or so, they stop being infectious.
How to reduce infection:
- Wash Hands Frequently
- Avoid touching your face and shaking hands
- Disinfect surfaces that are regularly touched
- Cover your face if you cough or sneeze
- Social distance - keep 1-2 metres between people
How to keep yourself healthy during the Coronavirus pandemic:
- Exercise daily – e.g. walking, cycling, gardening, yoga, tai chi
- Eat healthily – with plenty of fruits and vegetables
- Rest and relax – and reduce stress
- Connect with communities - friends and family via telephone and social media
- Stop smoking and drink alcohol in moderation - as these decrease immune responses
Treat symptoms with paracetamol, rest and drink regular fluids. Currently there is no cure, and a vaccine will take between 12-18 months before it is available. Traditional home remedies for colds, coughs and fevers may also help to relieve symptoms. Older or malnourished people may benefit from multivitamins and micronutrient supplements as protective measures.
WHO Q and A on Coronavirus:
https://www.who.int/news-room/q-a-detail/q-a-coronaviruses
YouTube, What Coronavirus Symptoms look like day to day – (from the WHO Joint mission to China):
https://mail.google.com/mail/u/0/#inbox/FMfcgxwHMPqxZLSnblwFKcQPlbMxxMQV?projector=1
Coronavirus the Science Explained; UK Research and Innovation: https://coronavirusexplained.ukri.org/en/
- Stop the Spread:
The most important principle to prioritise is to stop the spread through basic public health measures. Expanding surveillance and monitoring through widespread testing and syndromic surveillance, has the potential to target control responses and prevent a widespread epidemic with consequent deaths and social and economic disruption. This is especially important for countries whose health systems may be overwhelmed by the epidemic and whose economies and social fabric are put at risk of becoming de-stabilised or there are significant security risks if the epidemic spreads rapidly.
Lessons can be drawn from several Asian Countries, including Hong Kong and Singapore, which following their experience of responding to the SARS outbreak in 2003, applied extensive public health measures to prevent the infection becoming a widespread pandemic. After the initial outbreak of SARS, it was successfully contained by syndromic surveillance, contact tracing with prompt isolation and targeted quarantine measures. The measures attributed to interrupting human- to human transmission, which effectively eradicated SARS.
Lessons from South Korea - With a population of 51 million, was one of the first countries affected by coronavirus after the initial outbreak in China and drew upon its experience in successfully eliminating the 2015 MERS outbreak within 2 months. At the outset of the Coronavirus outbreak, it was able to design and create a test, and roll out a network of 96 laboratories across the country within 17 days, enabling 10,000 tests per day (5,200 per million population). This approach combined with rigorous contact tracing and quarantine, has managed to largely contain the epidemic, which peaked at the end of February, and to significantly minimize deaths (approximately 150 deaths at the end of March). By taking such swift action at scale, they have been able to avoid stringent lockdown measures, with less interference on their economy or on civil liberties. Social distancing is observed, people work remotely and schools have closed, however travelling has not been restricted, and city centres are already starting to reopen. https://coronavirusexplained.ukri.org/en/
The COVID-19 pandemic has significantly surpassed that of the SARS outbreak. However, the same principles can and have been applied to protect individual countries and communities, and reduced the overall peak of the epidemic, thus saving numerous lives.
Lessons from Asia – How to Stop the Spread
Lesson one: Take it seriously - and act quickly
Lesson two: Make tests extensive, and affordable
Lesson three: Trace and isolate
Lesson four: Early social distancing
Lesson five: Keep the public well informed and on side
https://www.bbc.co.uk/news/world-asia-51970379
Unfortunately, many European countries and the USA, have responded slowly to the risks of the COVID-19 Pandemic, and lost valuable time in stopping the spread with basic public health measures. This in turn will result in unnecessary harm and wider social and economic impacts that could potentially be avoided by swift action in other countries. The below chart outlines the trajectory of China’s outbreak compared to that of Italy by way of illustration to the importance of bringing in key public health measures swiftly to prevent the epidemic from spreading. By 19th March, China appears to have no new cases – except for those that are imported, and currently plans to lift community quarantines in April after a 3-month period of lockdown.
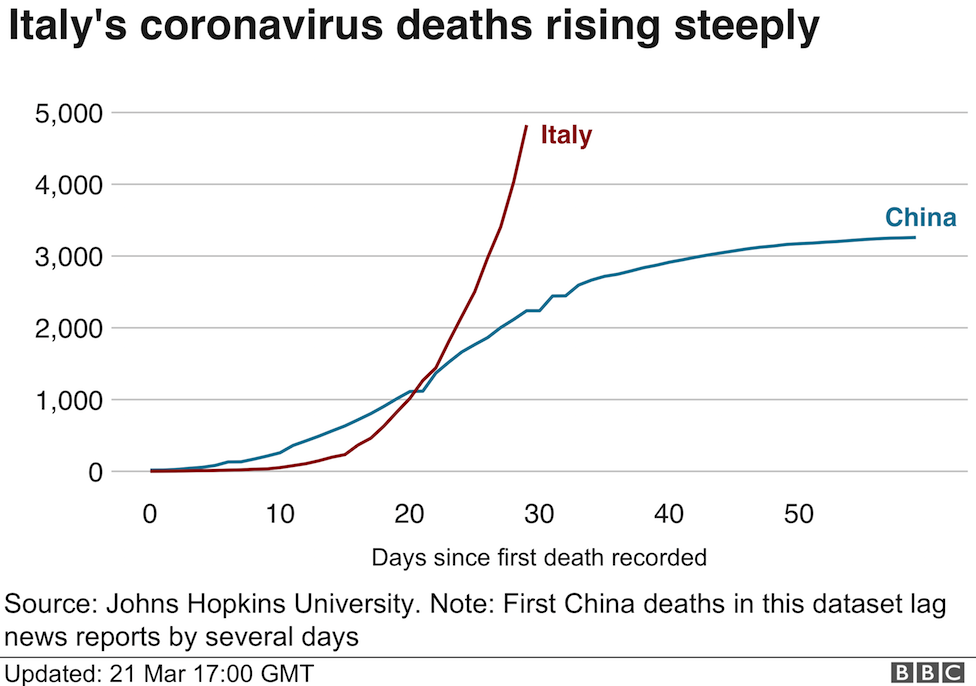
https://www.bbc.co.uk/news/world-europe-51991972
Surveillance and Monitoring:
Extensive Testing & Syndromic Surveillance - is key to allowing a country or community to appreciate what stage they are at, to apply targeted and appropriate measures. Without this information, responses are limited to reacting to hospital admissions – by which time the services will become easily overwhelmed. Many countries are producing their own tests in order to ensure testing of those with symptoms and their contacts, healthcare workers, as well as widespread community testing to provide a comprehensive picture of the epidemic.
Where tests are not sufficiently available, syndromic surveillance can be utilized – (see Annex 2 for a chart on comparative symptoms and Lessons from Sri Lanka below re digital surveillance tools). This approach relies on estimating numbers of patients seeking advice from healthcare centres, helplines or searching on websites, those who meet key symptoms related to COVID-19. This approach was successfully used to control the SARs epidemic.
Lessons from China: Clinical signs that can be adapted for syndromic surveillance:
Typical signs and symptoms include: fever (87.9%), dry cough (67.7%), fatigue (38.1%), sputum production (33.4%), shortness of breath (18.6%), sore throat (13.9%), headache (13.6%), myalgia or arthralgia (14.8%), chills (11.4%), nausea or vomiting (5.0%), nasal congestion (4.8%), diarrhea (3.7%), and hemoptysis (0.9%), and conjunctival congestion (0.8%).
Lessons from Sri Lanka - Digital Surveillance tools and applications:
COVID Shield™: The primary function of the App is to assist those who have been exposed and require or are in self-isolation/quarantine by offering a simple method to report symptoms, psychological status, social needs and location information. The App was created in Sri Lanka by the Commonwealth Centre for Digital Health along with partners and is intended as a common good to assist in the global response to COVID-19. The App can be used by other governments, corporations or any organization to provide services to those who are in quarantine and to implement quarantine processes effectively. For further information see: https://covid.iq.lk/covid-shield-app.php
Digital Surveillance Tool: DHIS2 has released a digital data package to accelerate case detection, situation reporting, active surveillance and response for COVID-19. The package is inspired by the Ministry of Health Sri Lanka’s pioneering design of DHIS2 tracker for COVID-19 case detection and draws on years of collaboration with the World Health Organisation (WHO) to develop information system standards for case-based disease surveillance. For further information and to download this free digital tool please visit: https://www.dhis2.org/covid-19
Trends: Information from tests and syndromic surveillance can be collated anonymously, with Digital Monitoring to inform trend analysis, modelling and projections. Where data on confirmed cases is lacking, the rate of deaths can provide information on trends. The WHO is monitoring a daily update on the outbreak, which is accelerating exponentially, and is now doubling in numbers every few days, for example, it took:
- 67 days from the first reported case of coronavirus to reach the first 100,000 cases
- 11 days for the second 100,000 cases
- Just four days for the third 100,000 cases
Model Risks: If no measures are undertaken within a country, the epidemic will peak within approximately 3 months from their first case. Death rates will be higher in countries with older populations and in those with weaker immune systems. Imperial College modelled potential outcomes for the UK and USA based upon different scenarios outlined below and in the graph:
- Do nothing – A high peak occurs within 3 months with 81% of the population infected and an estimated 510,000 deaths in the UK and 2.2 million in the USA; intensive care beds would be 30 times greater than availability.
- Mitigation – By isolation of those with symptoms and social distancing of vulnerable groups in order to slow the epidemic and flatten the curve – this reduces the impact upon the health sector by two thirds and halves deaths.
- Suppression – Aims to reverse epidemic growth, by eliminating human-to-human transmission, to flatten and reduce the curve through isolation and quarantine measures, mass social distancing and closure of educational institutions.
Projected critical care cases over time, according to different interventions
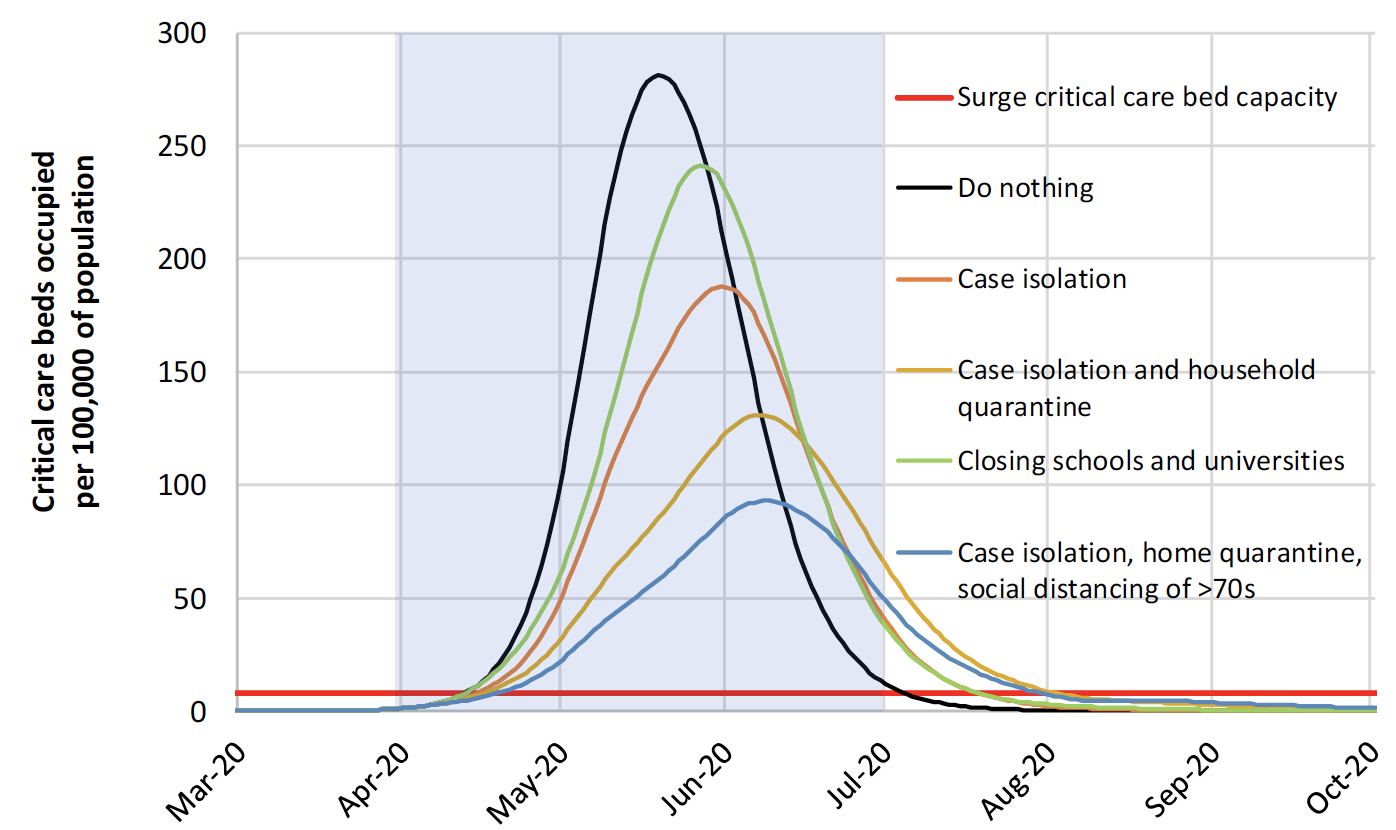
Note: Mitigation strategy scenarios for GB showing critical care (ICU) bed requirements. The black line shows the unmitigated epidemic. The green line shows incorporating closure of schools and universities; orange line shows case isolation; yellow line shows case isolation and household quarantine; and the blue line shows case isolation, home quarantine and social distancing of those aged over 70. The blue shading shows the 3-month period for interventions. https://www.imperial.ac.uk/media/imperial-college/medicine/sph/ide/gida-fellowships/Imperial-College-COVID19-NPI-modelling-16-03-2020.pdf
Contain and Control:
The aim of Containment and Control measures is to keep ahead of the epidemic curve and stop the spread of human-to-human transmission with the potential to eliminate the virus. Strategic surveillance and monitoring allows targeted control measures to contain and ideally supress and eliminate the epidemic within a population. This approach has been especially successful in many of the Asian countries, especially when they were instigated early and swiftly at scale.
However, as we can see from China, they have successfully applied these basic public health measures to reduce the overall impact of the epidemic even when it had spread into the community. Enhanced surveillance is especially required during this time to inform when community quarantine measures can be lifted and to identify any cases after the quarantine has ended. With rigorous surveillance and targeted containment, this approach has the potential to eliminate transmission, however the key challenge is the ability of this virus to spread before symptoms develop or when they are mild. We need to watch, learn and apply successful responses from Asia and China.
Lessons from China – containing an epidemic at population level
China’s uncompromising and rigorous use of non-pharmaceutical measures to contain transmission of the COVID-19 virus in multiple settings provides vital lessons for the global response. This rather unique and unprecedented public health response in China reversed the escalating cases in both Hubei, where there has been widespread community transmission, and in the importation provinces, where family clusters appear to have driven the outbreak.
Containing and controlling an emerging epidemic can be achieved by a robust and co-ordinated approach to the following activities:
- Contact Tracing: Identifying all at risk contacts of a positive case, testing them and instigating self-isolation or quarantine measures. Aside from the public health workforce, some countries have utilized CCTV, mobile phone tracking, detectives, the police or army to trace contacts, and used mobile alerts to inform at risk people.
- Hygiene: Basic measures such as hand-washing, providing hand sanitizers and regular cleaning with disinfectants to clean hard surfaces and handles. Focusing on vulnerable populations is especially important and some countries have provided additional water supplies and sanitizers to slum areas.
- Masks: The evidence re the effectiveness of facemasks in general is limited, and once they are damp, they can potentially increase the risk of infection, especially if removed incorrectly. Within a community setting, they are recommended for stopping the spread if worn by someone with an infection. However, as the infection appears to spread before symptoms emerge, and in order to reduce discrimination, some countries have mandated that everyone wear a mask in a public setting. Within this context, they may be an important barrier to slowing and stopping widespread community infection, especially within crowded communities that are less able to maintain social distance. Where there are shortages of masks, they should be prioritized for health and care workers who have extensive exposure.
- Isolation and Quarantine: Ideally, self-isolation for a period of 14 days is recommended to contacts identified, with an emphasis on an individual’s sense of responsibility to the wider community and to high-risk groups. In contrast, quarantine measures have a substantial impact upon an individual’s rights, by providing legal powers, where necessary, to contain an individual or group who are at risk of spreading the virus – for example, as has been used with cruise ships or with specific geographical areas or cities.
- Ports & Travel: Strengthening screening measures (temperature and screening questions) at ports, along with limiting travel, can assist in limiting mixing of infected individuals with non-infected populations, and therefore have a role in limiting the spread of the virus.
- Work from home: Where feasible, in order to reduce person-to-person transmission, measures should be put in place to enable people to work from home. The enhancement of bandwidth along with technological support in many countries has helped to maintain business continuity.
- Close educational institutions: Although children and young people are at less personal risk if they contract COVID-19, they are likely to increase the spread as they continue to mix with each other and their families with mild or minimal symptoms. In order to minimize inadvertent harm from closing educational institutions, guidance on limiting contact with older family members, or those with health problems is recommended. Some countries have provided schooling and childcare to allow essential workers to continue working.
Mapping websites:
WHO Situation Dashboard – Numbers by Country: https://experience.arcgis.com/experience/685d0ace521648f8a5beeeee1b9125cd
Lessons from China – the success of rigorous contact tracing
China has a principle of early identification, early isolation, early diagnosis and early treatment. Early identification of suspect cases is critical to containment efforts and occurs via a process of temperature screening and questioning at entrances to many institutions, communities, travel venues (airports, train stations) and hospitals. China has a policy of meticulous case and contact identification for COVID-19. For example, in Wuhan more than 1,800 teams of epidemiologists, with a minimum of 5 people/team, are tracing tens of thousands of contacts a day.
John Hopkins University Global Map of the Pandemic:https://www.arcgis.com/apps/opsdashboard/index.html#/bda7594740fd40299423467b48e9ecf6
Challenging environments: A key priority is to identify and intervene early in high-risk communities with crowded high density living of vulnerable populations, such as slums, refugee camps, care homes and prisons. These high-risk communities should have enhanced basic public health measures, combined with extensive surveillance and monitoring to be able to contain and control any infections early on. Some countries have released prisoners early to reduce overcrowding, and others have rapidly improved basic sanitation measures in slum and refugee camps.
Lessons from Jordan
Jordan is home to approximately 750,000 refugees, mainly from Syria, living in refugee camps and urban areas. With little capacity to respond to a major outbreak in their health systems, they prioritized basic public health measures to stop the spread of COVID-19 across their country.
Following the first case of COVID-19 in late January, local authorities acted swiftly to quarantine and contain patients and contacts. Airports and borders were monitored, and following an influx of infected visitors fro65m Italy, in March the government implemented a curfew and closed its borders, and subsequently imported 200,000 test kits. Officials proactively tested, contact traced, and quarantined and treated infected cases. Targeted community and city quarantines complemented this strategy, followed by random testing across the country to monitor community transmission. The government provided daily information on each case, regarding the location, mode of infection and action taken for each new case.
According to Jordan’s Ministry of Health (MoH), as of 17 April, there were 402 confirmed cases of COVID-19, with 250 individuals discharged from hospitals, and 7 deaths. Jordan’s experience demonstrates how, by focusing on early risk assessment, migration, effective communication and government-citizen co-operation, the pandemic can be managed.
https://www.linkedin.com/pulse/covid-19-how-did-jordan-rise-above-storm-moneef-zou-bi-phd/
Save Lives – the Health Sector Response:
The previous SARS epidemic in the early 2000s was effectively contained and eliminated through the above traditional public health measures that stopped all human-to-human transmission. Although a more severe disease with a higher fatality rate than COVID-19, it spread less easily, which made it more straightforward to contain. Additionally, COVID-19 appears to be most infectious in the early stages of the illness, when symptoms are mild or asymptomatic. This, along with a relatively complacent Public Health response in some countries has allowed the outbreak to spread across communities. In these situations, countries are essentially reacting to the outbreak as it unfolds and ramping up the health sector response through mitigation measures.
WHO Strategic Objectives re the COVID-19 Pandemic:
- Interrupt human-to-human transmission including reducing secondary infections among close contacts and health care workers, preventing transmission amplification events, and preventing further international spread*;
- Identify, isolate and care for patients early, including providing optimized care for infected patients;
- Identify and reduce transmission from the animal source;
- Address crucial unknowns regarding clinical severity, extent of transmission and infection, treatment options, and accelerate the development of diagnostics, therapeutics and vaccines;
- Communicate critical risk and event information to all communities and counter misinformation;
- Minimize social and economic impact through multisectoral partnerships.
*This can be achieved through a combination of public health measures, such as rapid identification, diagnosis and management of the cases, identification and follow up of the contacts, infection prevention and control in health care settings, implementation of health measures for travellers, awareness-raising in the population and risk communication.
Countries that have allowed the coronavirus to spread widely across their communities will reach a high peak of the epidemic within 3 months of their first case. Even at this stage, proactive and more aggressive community containment measures can assist in mitigating overwhelming health systems and the resultant high number of deaths. At this stage, key learning from China includes the importance of scaling up rigorous surveillance with testing, and subsequent targeting of containment and control measures in order to mitigate the impact and minimise overall harm. This is described as “flattening the curve” and can be illustrated in the below graph.
European objectives of community mitigation measures in a scenario of widespread community transmission of COVID-19 (European CDC 2020)
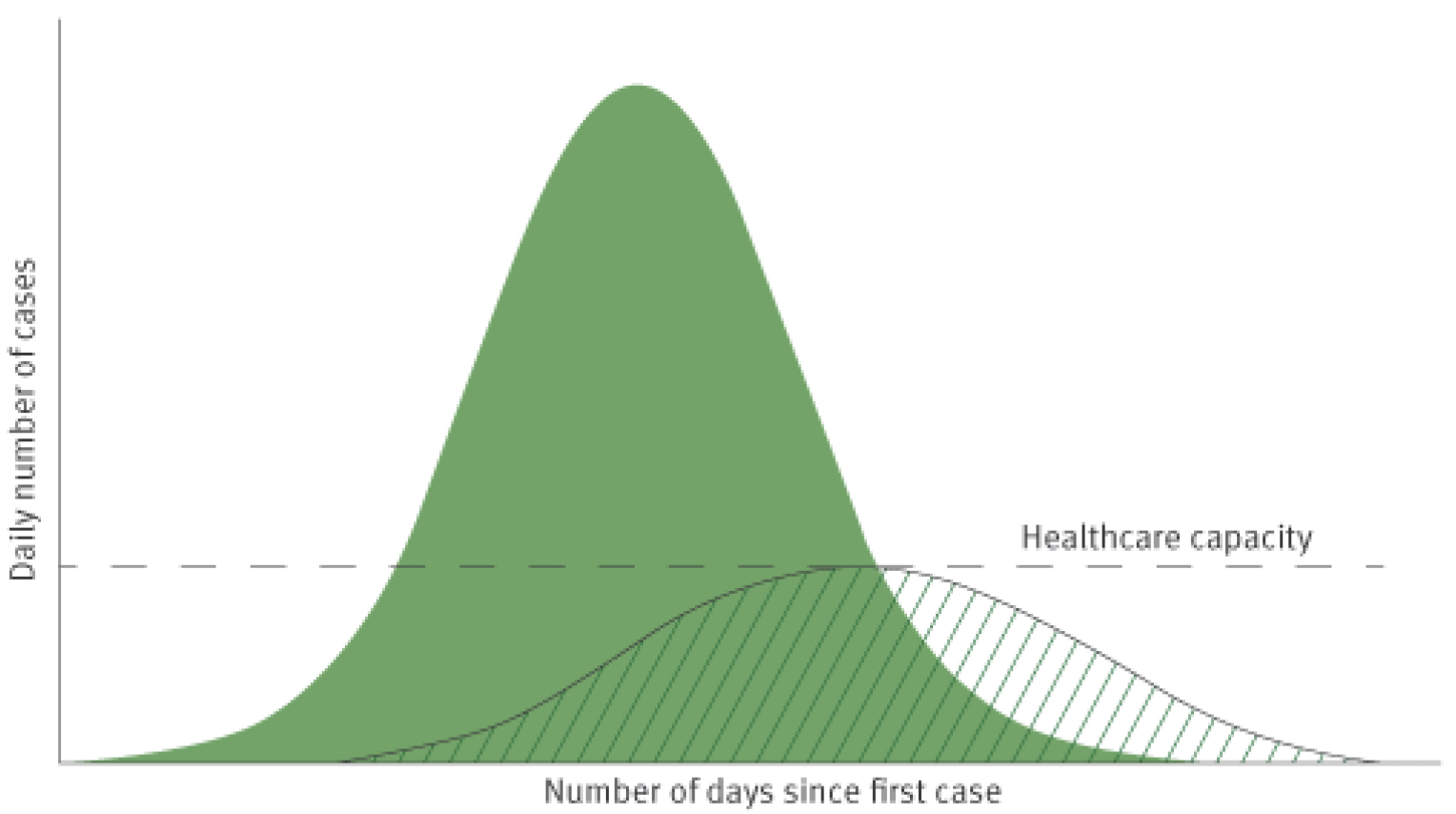
For countries at an earlier stage of the epidemic – a key lesson is to be proactive and get ahead of the curve by scaling up public health measures in order to avoid widespread community infections, with its subsequent avoidable deaths and impact upon civil liberties, societies and the economy. This is especially important for countries with weaker health systems, social capital and economic reserve. Even in high-income countries, the number of patients requiring intensive care treatment is estimated to be 30 times that compared to availability.
Estimated proportion of hospital admissions and fatality rates, including critical care requirements per age group based upon High Income settings
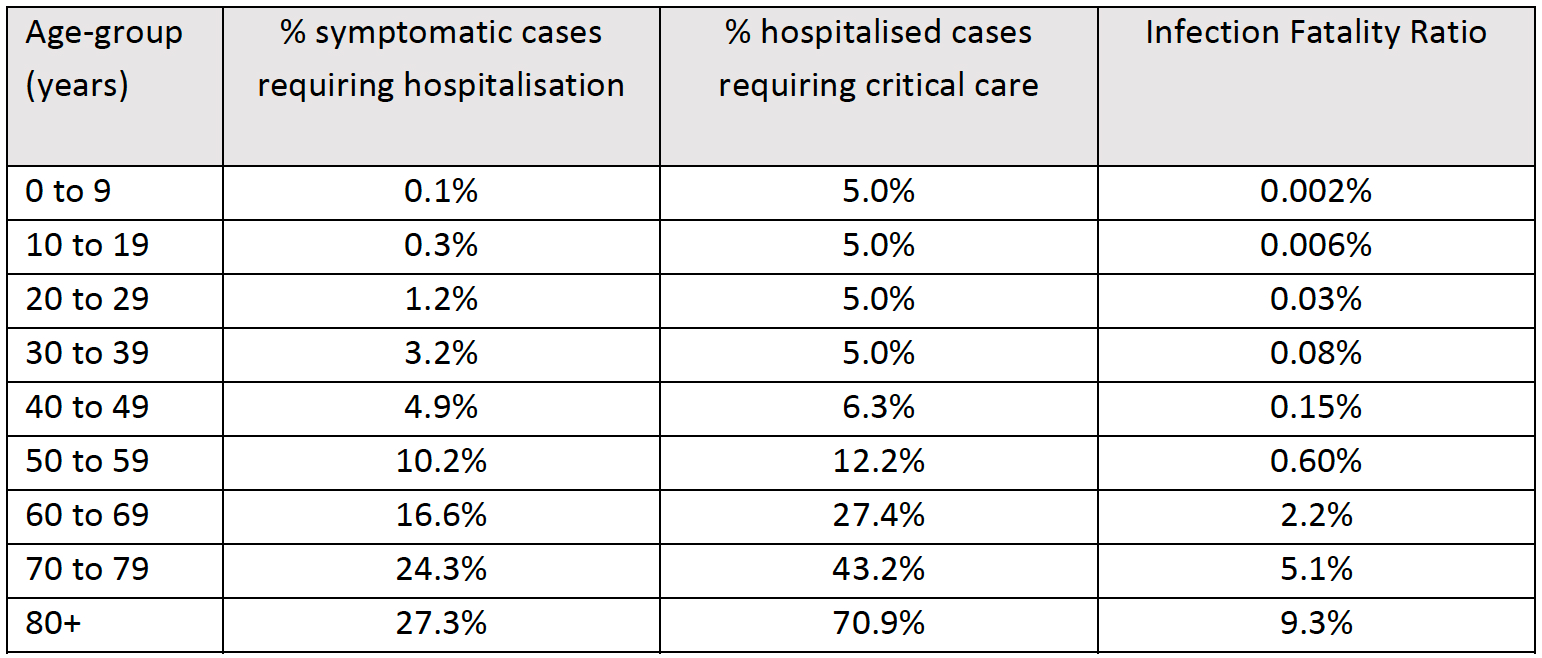
Even with mitigation efforts such as social distancing and community quarantine, curfews and social lockdown, the peak in intensive care requirements are likely to be 10-fold more than availability. The above table, from the Imperial College modelling, provides data for countries to estimate their anticipated health system response.
As the epidemic unfolds, precious time should be utilised to estimate and scale up the required health sector response, including the following areas:
Triage systems: with online websites and emergency helplines with syndromic checklists and symptoms requiring hospitalization. Ideally these systems collate anonymous data to inform demographic and geographical trends as part of the surveillance and monitoring of the outbreak.
Surge capacity: Needs to be estimated for the workforce (including the impact of sickness), for example by bringing in retired health care professionals and students, security forces and volunteers. Creating makeshift hospitals and beds, for example by creating tent-hospitals, commandeering hotels and private sector facilities; and scaling up the development and availability of tests, respirators and protective equipment.
Protect Health and Care Workers: Provide Personal Protective Equipment and establish phone and digital consultations. Ensure daily syndromic screening and prioritise COVID-19 tests for health and care workers, in order to protect their health and that of the patients they are treating. Additionally, test household contacts with symptoms –and quarantine health and care workers for 14 days - unless the household contact has a negative test.
Note: The incubation period means that a negative test for a health-worker living with a symptomatic person does not mean that they will not succumb to the illness, and as the period of highest infectivity is early on, they could still pose risks to patients. Testing for antibodies in Health and Care workers provides useful information on whether they have had the infection and are therefore likely to be resistant, as well as posing a low risk to patients.
Clinical Protocols: Share and learn from successful countries that have intervened early with clinical responses that have reduced the death rate and avoid patterns that have led to high fatality rates. Create ethical guidelines to enable compassionate decisions and care. Communicate about early successes regarding the application of established treatments to that of coronavirus, with a focus on early interventions that promote immunity and limit the more severe health outcomes.
WHO information on clinical guidelines:
Protect and Promote Mental Health: the pandemic is creating significant stress to different sectors of the population – ensure that helplines, web-resources, health and care workers, mental health services and community-wide approaches to address:
- Health and Care Staff – Post Traumatic Distress Syndrome, anxiety and guilt
- Patients in Hospital – re isolation from family, fear and distress of dying alone
- Community Isolation – of those living alone and with existing mental health illnesses, as well as increased fear and anxiety in the general population.
Mortuaries and Funeral Services: Based upon the anticipated mortality rates, scale up the provision of temporary mortuaries. Develop guidance to enable continued delivery of compassionate funeral services, whilst maintaining social distancing, for example, by holding outdoor or on-line services followed by plans for memorial services in the future.
Deliver Digitally: In order to protect health workers as well as other patients, the pandemic has in many settings resulted in a fast transformation to scaling up digital health responses. For example, by providing remote consultations, via telephone, online or via video consultations. This will potentially enable the more widespread digital transformation for delivering health systems in the future.
Clinical options and outcomes: Currently, the main clinical response is through supportive and critical care measures to address respiratory and multiple organ failure. Anti-viral medications and those that enhance immunity may also be beneficial; whilst other routine medicines may exacerbate clinical outcomes. Cures or preventative measures like vaccines do not as yet exist. The below figure provides a summary from the experience of the outbreak in China, with the estimated clinical progression and outcomes over time.
Lessons from China – Outcomes of clinical manifestations and hospital requirements over time
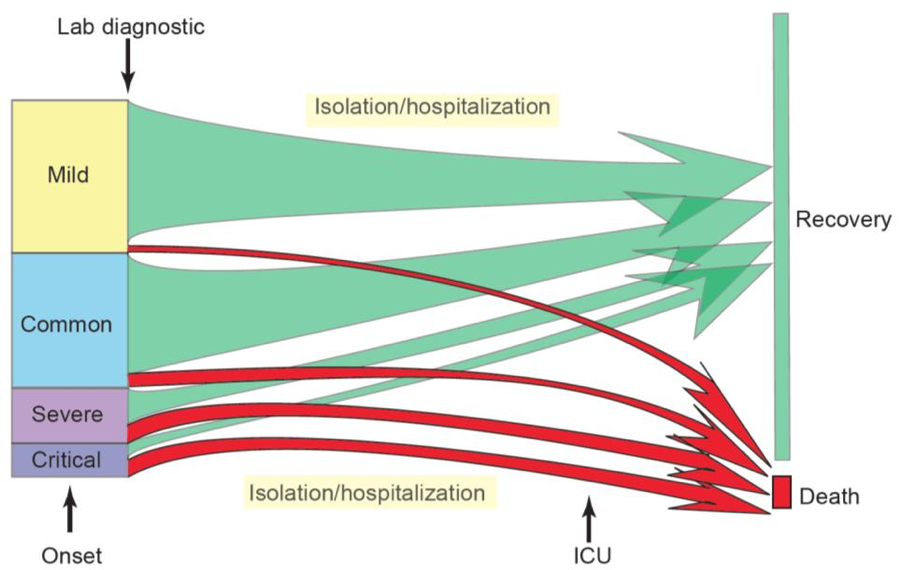
Note: the relative size of the boxes for disease severity and outcome reflect the proportion of cases reported as of 20 February 2020. The size of the arrows indicates the proportion of cases who recovered or died. Disease definitions are described above. Moderate cases have a mild form of pneumonia.
Using available preliminary data, the median time from onset to clinical recovery for mild cases is approximately 2 weeks and is 3-6 weeks for patients with severe or critical disease. Preliminary data suggests that the time period from onset to the development of severe disease, including hypoxia, is 1 week. Among patients who have died, the time from symptom onset to outcome ranges from 2-8 weeks.
- Protect and Secure:
Create Caring Communities:
In response to the strict social control measures that need to be applied to slow and stop the spread, it is important to emphasise our responsibilities towards other people in our community. Moreover, calling upon the good nature of individuals, communities and organisations can assist in transforming the experience of this pandemic to one of an infringement of freedoms, to that of the creation of compassionate communities.
Protect vulnerable populations: Identify high-risk groups to isolate, including older people and those with chronic conditions such as Respiratory disease, Diabetes and Cardiovascular disease, or with suppressed immune systems, for example due to cancer treatments. Additionally, malnutrition or obesity is likely to increase risk. Establish ethical guidelines to ensure compassionate responses exist for vulnerable groups. In particular, target interventions such as volunteering, telephone or online support, to those living on their own and for those whose mental health may deteriorate during extended isolation to contain the outbreak.
Lessons from China – High Risk Groups to Protect:
Mortality increases with age, with the highest mortality among people over 80 years of age (21.9%). The mortality rate is higher among males compared to females (4.7% vs. 2.8%). While patients who reported no comorbid conditions had a mortality rate of 1.4%, patients with comorbid conditions had much higher rates: 13.2% for those with cardiovascular disease, 9.2% for diabetes, 8.4% for hypertension, 8.0% for chronic respiratory disease, and 7.6% for cancer.
Community Connection & Support: Governments and communities can facilitate a positive response by emphasising that ‘we are all in this together’ and calling upon neighbours to support each other, as well as organising volunteer programmes. For example, the UK has managed to recruit over 500,000 volunteers to support the health services and provide community responses. Additionally, the private sector can enable families, friends and communities to stay connected by enhancing access to digital and internet services.
Public events & spaces: Learning from the successes of China, a number of countries have postponed public events and closed public spaces, including shops and the gathering of groups in order to minimize the spread of the coronavirus. Instigating such measures early on within a country’s epidemic potentially provides valuable time to allow countries to slow the spread, aided by rigorous contact tracing and testing to contain the outbreak.
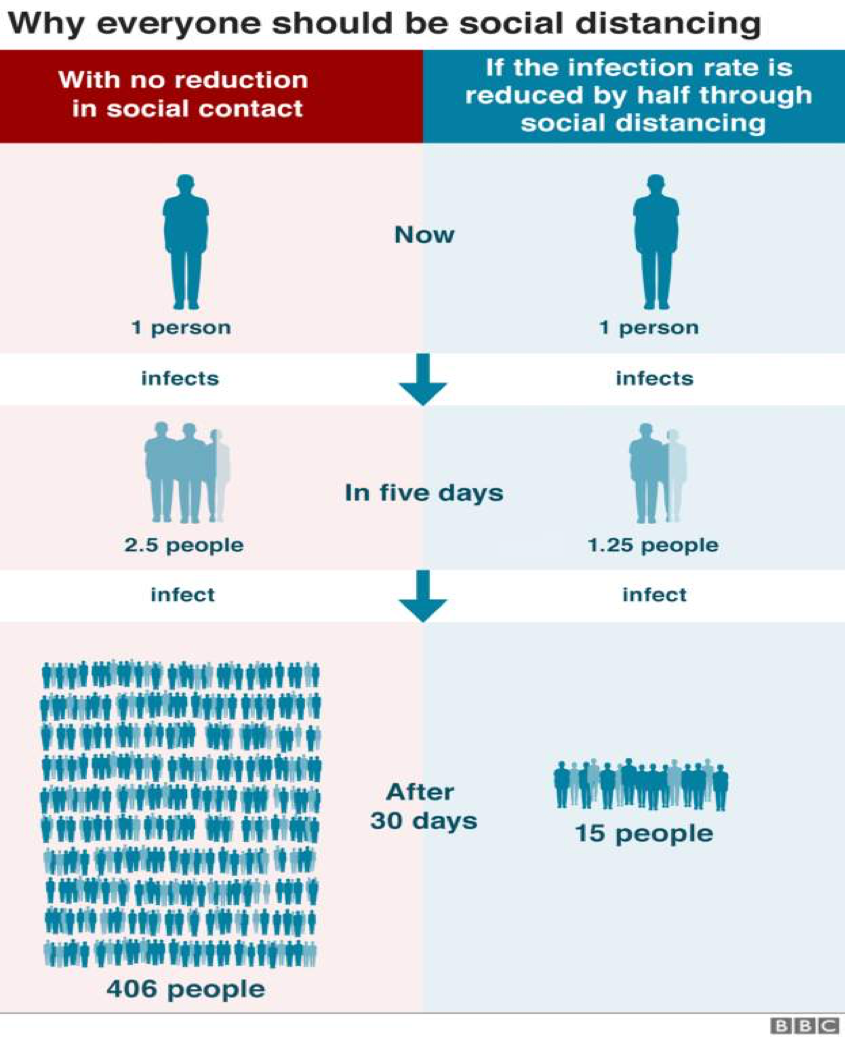
Social distancing: The main principle behind social distancing is to reduce the numbers who are infected and to slow and stop the spread – with a particular focus on protecting vulnerable people. Recommendations for social distancing vary from keeping a distance of 1-2 metres between people. Ensure that such control measures are proportionate to the spirit of the principles required. Some countries continue to allow daily walks or exercise near to their homes, as long as they observe social distancing restrictions, in order to promote a more resilient and healthier population. When applied at scale, this can be a very effective measure for controlling the spread of the epidemic, as visualised below:
Lessons from the Spanish Flu:
At the eve of the 1st World War, in 1918, the Spanish Flu emerged and spread rapidly around the world. In total an estimated one third (500 million) of the world’s population became infected with death rates estimated at 50 million – more than from WWI itself. There were three main waves of the epidemic over an 18-month period. At this time, the population was vulnerable from malnutrition, vaccines and medicines did not exist, and health services were minimal. To protect themselves and limit the impact, some communities were successfully able to apply a range of Public Health measures, including isolation, quarantine, hygiene, and limitations of public and social gatherings.
https://www.cdc.gov/flu/pandemic-resources/1918-pandemic-h1n1.html
Act Swiftly to Minimise Avoidable Harm: The more that the epidemic has been allowed to spread within a community, the more draconian the measures often need to be, including strict ‘lockdowns’ and curfews to keep people in their homes. The later such measures are implemented, and the more the epidemic is allowed to spread within a community, the longer community quarantines and lockdowns have to take place. Not only does this infringe more upon human rights, but also a delayed response increases the likelihood of the outbreak returning in further waves once the lockdown is lifted. Moreover, delayed responses will more significantly impact the economy, social stability and will needlessly result in larger numbers of potentially avoidable deaths. These will result from the Coronavirus itself, as well as an increase in additional risks related to reduced access to healthcare for non-coronavirus illnesses, as well as increased stressors related to the socio-economic disruption caused.
Stability and Security:
A key responsibility of government - is to ensure security across its populations, including maintaining the stability of essential services. In particular, creating a lockdown situation for a prolonged period of time has the potential to negatively impact upon income, food and housing security, economic growth and social security. Aside from the increased levels of worry about the coronavirus itself, a significant proportion of any population, will suffer from undue stress and anxiety regarding these fundamental factors required for daily living.
Communicating clearly and regularly about the rationale, key principles and the anticipated exit plan, are important elements to create a sense of certainty and stability. Additionally, this needs to be reflected in security measures that are proportionate for maintaining these principles and delivered in a way that encourages a sense of goodwill and community responsibility. Heavy-handed security measures during a lockdown potentially risk significant disquiet and unrest within a population, along with breaking down trust and instilling a negative relationship with the Government.
By ensuring a sense of safety, stability and hope, will also be key to the resilience of communities and their ability to pull together and recover in a positive way from this pandemic. Below provides an outline for areas that need particular consideration for maintaining a sense of security and stability.
Essential Services including Food Security - Establish a multi-sector group to identify essential public and private services, map for delivery continuity processes and potential risks to a breakdown across these often-interrelated systems. Pay particular attention to essential services, including food supply, water and sanitation, energy, essential travel and communications. Establish regular food delivery systems, including free food and food banks, targeted at populations that are most vulnerable to the impacts of a lockdown. Consider rationing of food to minimize panic-buying of supplies and to ensure a fair and even distribution. Identify key workers across the public and private sector, and put in place mechanisms to allow business continuity, with an emphasis on supporting the health sector. Engage volunteers and young people in agricultural activities and harvesting in order to maintain food security.
Stability of Education, Income and the Economy – This pandemic has led to the closure of schools and educational institutions in many countries to reduce the spread of the infection. In order to limit the impact upon future opportunities for young people, it is important to maintain continuity of distant education, for example through public radio, television or through online lessons and webinars. Identify fiscal measures to stabilize the economic impact for the country as well as for individuals and communities. For example, put in place postponement systems for taxes, bills and debts; create rapid loans for Businesses and Small to Medium Enterprises; and provide income support for workers no longer receiving an income and those on lower incomes. For example, some countries are providing universal credits, handouts or up-to 80% of prior income to prevent households falling into poverty. The private sector can be actively engaged to develop solutions and put plans in place, which can also facilitate the recovery process, as outlined in the example below.
Lessons from Kenya – Engage the private sector to stabilise economic impacts
The Kenyan Government aims to keep ahead of the epidemic curve. Therefore, within the first 12 days of its first case, it has announced a series of measures to reduce fear and enhance stability and security. These are in addition to instigating basic public health measures to stop the spread of infection. They include measures such as income support, tax relief, and benefits to vulnerable populations. Additional funding is being released to recruit further health workers. Within the context of a strong cultural ethos of everyone pulling together in a crisis, the Kenyan Private Sector Alliance released detailed plans to mitigate the economic impacts of the outbreak, as well as to support maintenance of essential services. This has been developed into a management framework based upon the below principles:
Economic Management Framework for the COVID-19 Response – key principles:
- Maintaining jobs and livelihoods;
- Prioritizing the health and safety of our employees, communities, and healthcare workers;
- Protecting Small to Medium Enterprises;
- Ensuring business and supply chain continuity;
- Mobilizing private sector capabilities and resources;
- Maintaining highest ethical standards;
- Avoiding moral hazard traps such as price spikes or producing or distributing lower quality products;
- Disseminating clear and accurate information frequently;
- Promoting social stability.
Source: The Kenya Private Sector Alliance - KEPSA
Housing and Social Security – Target those at most risk, for example those living in slums and crowded homes, for example, some countries have provided water supplies to slum areas, hotel accommodation for homeless populations. Adopt rapid legislation to protect defaults on rents and mortgage payment, so that people are not made homeless due to lack of income. Ensure basic waste disposal and sanitation services, targeting crowded populations by providing soap, water and disinfectants.
Security Services – Provide rapid protocols and training of the police and army, to enable them to enforce emergency legislation and act as surge capacity for managing the emergency response. Utilise CCTV, social media, community and neighbourhood reporting to act swiftly on emerging ‘scams.’ Establish specialist teams, with telephone and online resources to address anticipated domestic abuse (which rose three-fold during the lockdown in China). Where necessary release non-dangerous prisoners. Draw upon retired and reserve forces to expand the workforce to support and provide essential services.
- Research, Recover and Reflect:
Research: Continuous evaluation and research during the pandemic is a key part of how we can constantly improve upon response and share effective outcomes. Therefore, ensure information collated from the surveillance and monitoring process is linked to demographic, geographical details and health outcomes, to enhance responsiveness and impact. Research institutions can also inform the government expert group with risk scenarios and future projections to inform planning and emergency responses. Research and evaluations are being collated by the WHO to facilitate shared learning during the course of the pandemic on the below web-link:
WHO – Collation of Research on COVID-19: https://www.who.int/emergencies/diseases/novel-coronavirus-2019/global-research-on-novel-coronavirus-2019-ncov
Where possible, invest in national and international research programmes to find solutions to address the coronavirus. For example, through preventative means, such as a new vaccine, anti-viral medicines, curative treatments and respirators. Additionally, research institutions can design and evaluate the effectiveness of delivering at scale, low cost aspects for Testing and Protective Equipment. Rapid international evaluations on the relative effectiveness of different country strategies to the pandemic can also inform future responses and recovery processes.
Vaccines and new medicines are likely to take 12-18 months to identify, develop and test for safety, before they are made available at scale. In the longer-term, we need to take greater heed of prior research recommendations to enhance our preparedness for future pandemics, including the WHO research recommendations of:
- Enhancing global coordination of all relevant stakeholders
- Support a clear and transparent global research
and innovation priority setting process - Build common platforms for standardized processes, protocols
and tools, as well as for sharing specimens, data, and information https://www.who.int/docs/default-source/coronaviruse/srp-04022020.pdf?sfvrsn=7ff55ec0_4&download=true
In 2016, the Commission on a Global Health Risk Framework for the Future recommended an accelerated approach to Research and Development to prepare for Pandemics. The Commission estimated that an additional $1 billion a year is invested into projects in drugs, vaccines, diagnostics, personal protective equipment, and medical devices, as well as in defining protocols and practical approaches.
Commission on a Global Health Risk Framework for the Future 2016; National Academy of Medicine, Secretariat:https://www.nap.edu/catalog/21891/the-neglected-dimension-of-global-security-a-framework-to-counter
Recover: Early on in the response process, it is recommended to establish a multi-sector Recovery Committee to feed into the National Emergency Committee. Ideally, senior leaders, who are not directly involved in the emergency response, will head this up. This will allow for strategic thinking to shape the response during a period of any lockdown or community quarantine, develop exit strategies and the longer-term recovery response. Possible exit strategiesinclude the below:
- Suppression and Early Elimination - of human-to-human transmission with continued surveillance and port controls – this approach is potentially feasible with rapid public health interventions, informed by extensive testing and contact tracing.
- Mitigation – of the health impacts by flattening and extending the epidemic curve, to allow health services to cope with the high level of cases. This approach can lead to many months of social controls and uncertainty, with extensive negative consequences upon the economy, social harmony and other health outcomes, including prolonged fatalities.
- Improve Clinical Outcomes - There is some scope of improving survival rates by sharing effective clinical protocols based upon the adaptation of existing treatments, regionally and internationally.
- Wait for Research Solutions – A vaccine presents a longer-term preventative solution, however there is no certainty that an effective vaccine will be found, and it will take at least 12-18 months to become available at scale. This is also true for potential new treatments.
- Do nothing – This approach will have the highest death rates, with significant social and economic impacts. Natural ‘herd’ immunity is likely to take an 18-24-month period to develop, as happened with the Spanish Flu.
Recovery and the Length of Lockdown: The experience of China releasing its lockdown after 3 months duration will help to inform the response in many countries. A late response leading to widespread community infection is likely to require a longer period of lockdown with a more extensive and costly recovery plan. For example, the WHO pandemic preparedness-monitoring group has estimated a drop by 5% of GDP resulting from a pandemic of this sort. More recent estimates suggest that the longer a lockdown, the more significant the economic losses, as businesses close and unemployment rises, and a longer-term recession. Late responders are also likely to experience recurrences of community infections, with further cycles of outbreaks and lockdowns. This will especially occur in countries that have undertaken minimal testing and are therefore unable to target their containment responses.
Lessons from China – Planning Recovery
China is already, and rightfully, working to bolster its economy, reopen its schools and return to a more normal semblance of its society, even as it works to contain the remaining chains of COVID-19 transmission. Appropriately, a science-based, risk- informed and phased approach is being taken, with a clear recognition and readiness of the need to immediately react to any new COVID-19 cases or clusters as key elements of the containment strategy are lifted.
The period of recovery will depend upon the swiftness of eliminating the epidemic. In those countries which enhance basic public health measures such as testing, contact tracing, quarantine and social distancing at speed and scale at the outset, then the period of social and economic interruption is likely to be a lot shorter. For example, early public health interventions across South Korea have resulted in a small peak of cases and deaths, with minimal social and economic disruption, for a relatively short duration.
SDG Continuity: Considerations need to include the potential impact upon progress towards the Sustainable Development Goals, including the economy, society and upon health. Include Government, public and private sector representatives, as well as processes to engage with communities. Identify potential and worst-case risk scenarios, in consideration with established government risk assessment plans so that solutions are not developed in isolation. In past recessions, countries that have injected significant investments to boost the economy and public services have tended to recover more quickly. This investment can potentially be directed to develop a green and digitally transformed economy in order to ensure longer-term sustainable development.
Build Back Green – and connect communities to create a new future together:
A key opportunity that arises from any catastrophe of this sort is that during the recovery process, there is the possibility to create a better future together. For example, this pandemic is creating a significant and rapid social, economic and digital transformation in the way that we do things. It is also enhancing volunteering and compassionate responses, with communities pulling together for a common good. The peace and quiet created by mass lockdowns also allow time for reflection and has been shown to reduce travel and pollution levels.
Additionally, it is generating creativity and enhancing a sense of global and community connectivity that could help us recover from this pandemic, as well as to find solutions to our wider global challenges such as the climate crisis. For Example, Nature Based Solutions have the potential to create more resilient communities that could also reduce the risk of emerging infections crossing over from animals to humans.
The World Bank comments on the opportunities of investing in Green Infrastructure as part of the Recovery Process, including renewable energy, low carbon infrastructure, and climate change adaptation. https://blogs.worldbank.org/governance/pandemic-unexpected-opportunity-climate-action
Moreover, in order to respond to the pandemic and support recovery, the World Bank Group has recently committed US$160 billion over the next 15 months to help countries protect the poor and vulnerable, support businesses, and bolster economic recovery.
Reflect: At the time, the lessons from the Ebola outbreak were seen as a global wake-up call – to address the multiple perceived failures to address such outbreaks. Although the Ebola outbreak was eventually contained, it was only after enormous efforts by the national and international communities, with substantial loss of life and economic costs. Both the costs and loss of life could have been significantly reduced if the following had been in place:
- Rapid surveillance and alert systems;
- The ability of health systems to respond;
- National and global co-ordination.
Following the Ebola outbreak, in 2016, the Commission on a Global Health Risk Framework for the Future reviewed the risks for pandemics, made recommendations to enhance preparedness and estimated costs to do so. In particular, they recommended strengthening global co-ordination and capabilities along with enhancing health security as a global public good and making public health a foundation of health systems. Many countries have fragmented health systems with minimal investment (often only 3-5%) of their Health Sector budgets spent on basic public health measures such as preventative and health protection services. They also recommended the development of a global framework to counter infectious disease crises. To fund this, they made the case to invest approximately $4.5 billion annually for pandemic preparedness. With the significant loss in the global economy and costs incurred to respond to the COVID-19 pandemic, this can be seen to be a minimal cost to pay for our health and global security.
Similar recommendations were also made by the WHO Global Preparedness Monitoring Board Annual Report in 2019, as part of the delivery for the Sustainable Development Goals. This called upon leaders to invest in their responsibilities in pandemic preparedness, including the full implementation of the International Health Regulations.Greater global and national multi-sector co-ordination was recommended, including for risk assessments, preparedness planning and response. There was also a recommendation that financial institutions incorporate pandemic preparedness into their risk assessments, and that donors enhance investment into pandemic preparedness.
In response to the Ebola outbreak the InterAction Council, a group of former heads of government and state, convened a series of high-level expert group meetings to identify the links between global security and the key health risks that threaten us. In our increasingly globalised world, there is an increasing risk from emerging infectious diseases and pandemics.
Additionally, the impacts of our climate and environmental crisis appear to act as drivers for the emergence of new infections and global disease outbreaks. This resulted in the development of a Charter for One Health, which emphasises the importance of linking the prevention of disease outbreaks with the urgency of taking action to address our planetary health emergency. The Charter was endorsed by former leaders at the InterAction Council Plenary session in Dublin, in 2017.
The main recommendations from this Charter, in relationship to the COVID-19 pandemic, are even more relevant today, and include the actions in the table below:
The InterAction Council Actions in the Charter for One Health (2017):
- Co-ordinated local, national, multilateral, and global solutions are required to tackle poverty, global environmental change, peace and justice, access to clean water, and responsible production and consumption.
- Increased resilience is needed to respond to emerging threats and to tackle the driving forces of environmental change in order to enhance the integrity of the natural systems on which humanity depends.
- Environmental health should be integrated into health budgeting with a preventive approach. There is an obligation to expand trans-disciplinary research to address gaps in knowledge through defining the links between health and environmental change, and to develop potential adaption strategies for populations subject to environmental change.
- There is an imperative that governance, accountability, monitoring and independent evaluation be improved and policy, legislative and regulatory changes will be necessary in all sectors related to health – social, economic and environmental determinants and patterns of international commerce, trade, finance, advertising, culture and communications.
- Fearless leadership is needed, as well as whole societal engagement, recognizing that governments acting alone will not be able to deliver One Health and will require broader leadership from civil society, the scientific community, academia, local government and the private sector supported by a global learning network.
- Establish an independent accountability mechanism to ensure monitoring and review of the aforementioned Actions for One Health.
http://www.interactioncouncil.org/34th-annual-plenary-meeting-concludes-dublin-charter-one-health
Reflections for the Future:
As tragic as this Pandemic is, it reveals humanity’s vulnerabilities as well as how interconnected we all are. Ultimately though, we will look back on this catastrophe as a wake-up call of our global responsibilities to prevent future pandemics, as well as in responding at speed to our impending climate and environmental crisis.
This sentiment is reflected in the letter below, developed in collaboration with the Club of Rome and the Planetary Emergency Partnership, and builds upon the InterAction Council ‘Manifesto to Secure a Healthy Planet for All – a Call for Emergency Action.’
Open Letter: Emerging from the emergency–One Planet, One Humanity, One Health
It is time to harness our fears, build hope and drive action to build resilient societies on the longer term.
The world has been plunged into an extraordinary crisis. We share a deep concern for the human cost COVID-19 is inflicting and express a profound sense of solidarity with the most vulnerable communities. We fully support the emergency measures needed to save lives and protect the economy.
This pandemic is teaching us how much we depend on each other for our health systems, food systems and supply chains. We are all on this planet together. And the planet is in the midst of a deeper and longer-term crisis rooted in a number of interconnected global challenges. Humanity has crossed planetary boundaries. International cooperation is the best option to resolve future existential threats. Like COVID-19, climate change, biodiversity loss, and financial collapse do not observe national borders. These threats must be managed through systemic and collective action. Countries are stronger together.
How leaders decide to stimulate the economy and allocate capital in response to the crisis will either amplify these threats or mitigate them. The risk is making near-sighted decisions that increase emissions and continue to degrade nature. It is time to invest in nature, phase out fossil fuels, move to a circular economy and accelerate the transition to resilient low-carbon economies.
We call on leaders to have the courage, wisdom and foresight to seize the opportunity to make their economic recovery plans transformative for people and nature. In so doing, they will secure a path to net zero emissions by 2050 to meet the Paris Agreement, transform our food systems and rebuild our relationship with nature. That is why it is so important that climate and biodiversity stay at the top of the agenda, and that leaders leverage every opportunity to keep up momentum and make progress at the United Nations nature, climate and biodiversity summits later this year.
This is the moment to rise to the challenge to emerge from this emergency with a global economic reset. Ensuring the health and prosperity of people and the planet is possible if we make bold decisions today so that future generations can survive and thrive in a better world.
A Global Call from the Planetary Emergency Partnership signed by 1,000 leaders and scientists from around the world https://www.climate-sustainability.org/planetary-emergency
Financial Times Letter: “We Call on Leaders to put climate and biodiversity at the top of the agenda” March 27, 2020: https://www.ft.com/content/09d934ac-6f59-11ea-9bca-bf503995cd6f
Initial Recommendations for Future Pandemic Preparedness and Emergency Responses:
- Build Back Green – As part of the recovery process, invest in solutions that address the climate crisis and enable progress towards the Sustainable Development Goals, including nature-based solutions, renewable energy, low carbon infrastructure, climate change adaptation.
- Enable the Digital Transformation – Continue the rapid digital shift during the pandemic to create connected communities that are able to share learning, find solutions and respond at scale to building back green; ensure digital governance to prevent misinformation, hacking and scams; and enhance efficient ways of working, with reduced travel, with the creation of digital health systems for Planet, Place and People for a common future for all.
- Courageous and Collaborative Leadership – For the wellbeing of future generations, in order to apply learning from the pandemic, re scaling up emergency processes and unified efforts to address the climate and environmental crisis; empower young people with the skills and experience required to address emergencies and to secure a healthy planet for all.
- Establish an Independent Global Emergency Mechanism – Tasked with enhanced surveillance and monitoring, risk assessment and detection, with rapid alert and response systems; such an organisation needs to be able to establish a global and multi-sector response at speed, communicate freely, have independent governance and be able to collaborate and mobilise action across the international community.
- Invest in Emergency Preparedness and Response – The Commission for a Global Health Risk Framework for the Future recommends an annual global investment of US$4.5 billion for pandemic preparedness, including public health preventative measures and research. Such an organisation could have wider responsibilities, including relevant aspects to address the Planetary Emergency.
- Strengthen Public Health and Health Protection – Invest in and enhance essential public health operations and services within every country– a weak link anywhere is a weak link for us all – ensure that this is embedded within national health systems to enable national, regional and local coordination and surge capacity during outbreaks.
- Enhance links with multi-sector emergency mechanisms – Ensure that health risks and planning, including for pandemics are incorporated across global, national, regional and local emergency planning systems and governance mechanisms – building upon the Sendai Framework for Disaster Risk Reduction.
- Increase Research into Prevention and Preparedness - The Commission for a Global Health Risk Framework for the Future recommends an annual global investment of US$1 billion for research into pandemic preparedness; investing in research on the effectiveness of preventative and health protection measures provides the most scope for reducing avoidable deaths, whilst maximising economic savings, and reducing global security impacts.
Further Resources:
Annelies Wilder-Smith, Calvin J Chiew, Vernon J Lee ‘Can we contain the COVID-19 outbreak with the same measures as for SARS?’ The Lancet, Published Online
March 5, 2020 https://doi.org/10.1016/ S1473-3099(20)30129-8; https://www.thelancet.com/action/showPdf?pii=S1473-3099%2820%2930129-8
Commission on a Global Health Risk Framework for the Future; National Academy of Medicine, Secretariat; National Research Council 2016. The Neglected Dimension of Global Security: A Framework to Counter Infectious Disease Crises. Washington, DC: The National Academies Press. https://www.nap.edu/catalog/21891/the-neglected-dimension-of-global-security-a-framework-to-counter
ECDC: Novel coronavirus disease 2019 (COVID-19) pandemic: increased transmission in the EU/EEA and the UK – sixth update, 12 March 2020:https://www.ecdc.europa.eu/sites/default/files/documents/RRA-sixth-update-Outbreak-of-novel-coronavirus-disease-2019-COVID-19.pdf
Hassan S, Sheikh F N, Jamal S, et al. (March 21, 2020) Coronavirus (COVID-19): A Review of Clinical Features, Diagnosis, and Treatment. Cureus 12(3): e7355. doi:10.7759/cureus.7355: https://www.cureus.com/articles/27924-coronavirus-covid-19-a-review-of-clinical-features-diagnosis-and-treatment
Nurse J, Dorey S, Yao S, Sigfid L, Yfantopolous P, McDaid D, Yfantopolous J, Moreno JM: ‘The Case for Investing in Public Health’ WHO Europe, 2014; www.euro.who.int/publichealth
Nurse J, Moore M, Castro A, Dorey S, Laaser U, (2016) ‘A Systems Framework for Healthy Policy – Advancing Global Health Security and Sustainable Well-Being for All’ Implementation Tool for the ‘Global Charter for the Public’s Health’; The Commonwealth Secretariat, London, UK; www.thecommonwealth-healthhub.net
Sandifer Q, Dorey S, Nnoaham K, Shankar G, Watson C, Eze E, Brunt H, Dukes G, Battersby S, Archer P, Gilhooly D, Singh A, Dissanayake V, Wyn-Owen J, Aylward M, McDonald B, Nunn R, Nurse J: ‘Health Protection Policy Toolkit: Health as an Essential Component of Global Security’; 2ndEdition; Public Health Wales and the Commonwealth Secretariat, 2017, www.thecommonwealth-healthhub.net
WFPHA (2016) ‘A Global Charter for the Public’s Health – the public health system: role, functions, competencies and education requirements’ The European Journal of Public Health, March 8, 2016; https://www.wfpha.org/images/PHAA01001_Global-Charter_PROOF_160812_FINAL.pdf
United Nations: Shared responsibility, global solidarity: Responding to the socio-economic impacts of COVID-19; 2020: https://unsdg.un.org/resources/shared-responsibility-global-solidarity-responding-socio-economic-impacts-covid-19
United Nations: The Secretary-General's UN Response and Recovery Fund for COVID-19; 2020: https://unsdg.un.org/resources/secretary-generals-un-response-and-recovery-fund
WHO: Global Preparedness Monitoring Board, Annual Report 2019 https://apps.who.int/gpmb/annual_report.html
WHO Technical Guidance for Coronavirus: https://www.who.int/emergencies/diseases/novel-coronavirus-2019/technical-guidance
WHO: Report of the WHO-China Joint Mission on Coronavirus Disease 2019 (COVID-19): 16-24 February 2020:https://www.who.int/docs/default-source/coronaviruse/who-china-joint-mission-on-covid-19-final-report.pdf
WHO Pandemic Influenza Checklist, 2018: https://apps.who.int/iris/bitstream/handle/10665/259884/9789241513623-eng.pdf?sequence=1
World Bank: ‘One Health - Operational Framework for Strengthening Human, Animal, and Environmental Public Health Systems at their Interface’ 2018: http://documents.worldbank.org/curated/en/961101524657708673/pdf/122980-REVISED-PUBLIC-World-Bank-One-Health-Framework-2018.pdf
Annex 1: The InterAction Council:
Is a group of former Statesmen established in 1983 by political world leaders. It consists of over 40 former Heads of State and Government and is presently co-chaired by HE President Olusegun Obasanjo from Nigeria and HE Bertie Ahern, former Prime Minister for Ireland. It creates recommendations and proposals for action on its main priority areas of:
- Peace and security
- World economic revitalization
- Universal ethical standards
The InterAction Council provides senior level strategic recommendations and guidance, convenes regional and international meetings to advocate for priority areas and facilitate country engagement. Key publications, communiques and declarations are circulated to heads of government, senior policy makers, opinion leaders throughout the world, as well as to international institutions.
Over the last few years, the Interaction Council has focused on global health security in response to the Ebola and Zika outbreaks, with a view to identifying policy responses that strengthen sustainable health systems and as part of a wider contribution to global security. The relevance of health to the climate change and sustainable development agenda has also been explored as part of this agenda, with a series of expert meetings. The culmination of this work has led to the development of the ‘Dublin Charter for One Health’, endorsed by the Interaction Council in June 2017, followed by the ‘Manifesto to Secure a Healthy Planet for All – A Call for Emergency Action’ in 2019:
The InterAction Council ‘Dublin Charter for One Health’ 2017: http://www.interactioncouncil.org/34th-annual-plenary-meeting-concludes-dublin-charter-one-health
The InterAction Council ‘Manifesto to Secure a Healthy Planet for All – A Call for Emergency Action’ 2019: https://www.interactioncouncil.org/publications/manifesto-secure-healthy-planet-all-call-emergency-action
Annex 2: Comparative Symptoms Chart for COVID-19:

Annex 3: COVID-19 and the Sustainable Development Goals:
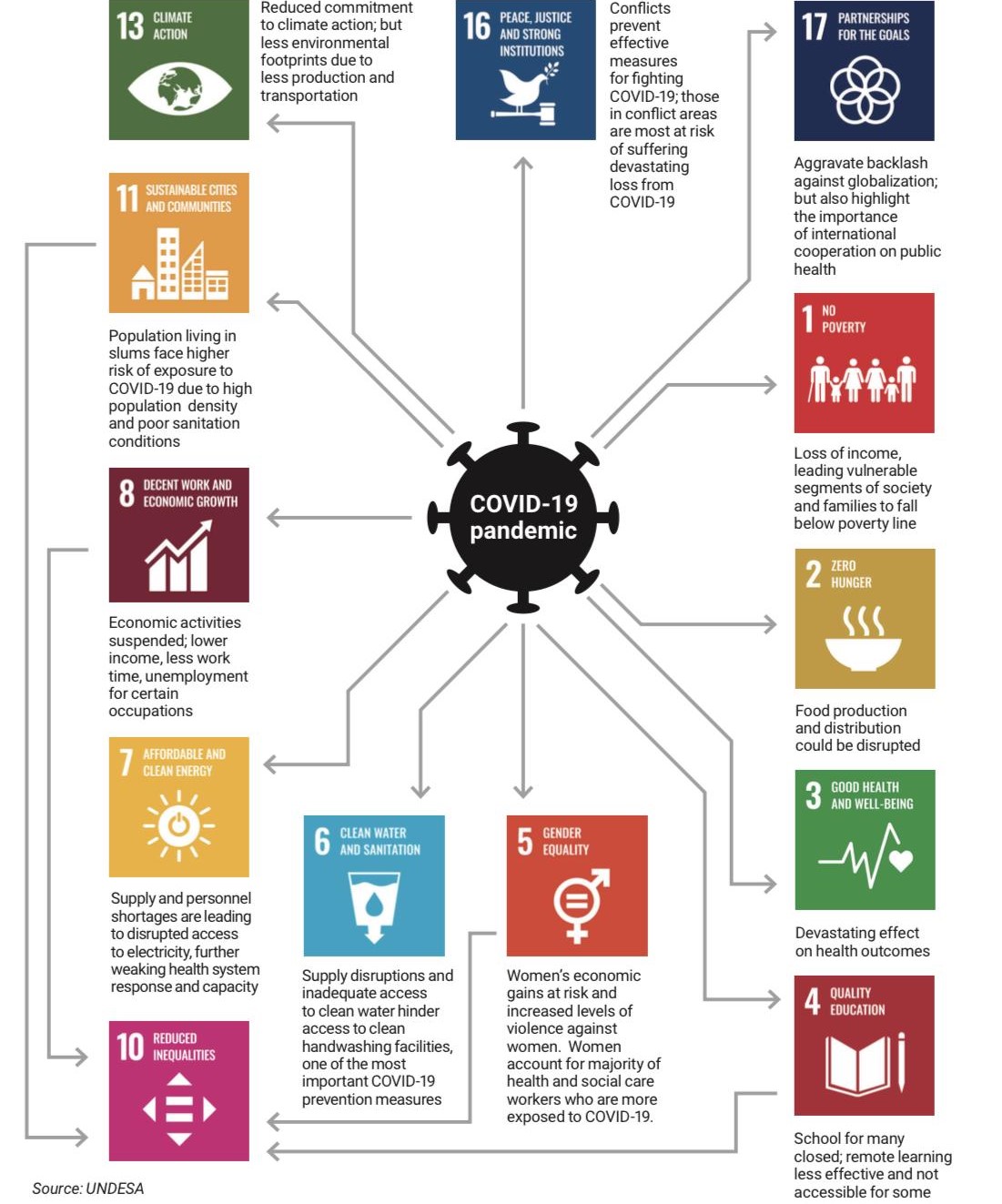
https://www.un.org/sites/un2.un.org/files/sg_report_socio-economic_impact_of_covid19.pdf
This Framework is endorsed and supported by the following organisations: